In my travels learning as much as I reasonably could to optimize my gender transition, I came upon a doctor named Will Powers infamous in certain trans circles for his unorthodox style. Dr. Powers takes it upon himself to do better than others who follow the ancient gender affirming treatment standards. He has some interesting ideas, makes himself available for questions on his sub-Reddit, and publishes presentations online that he gives to doctors interested in serving trans patients.
While I’m skeptical of a number of things he has to say and the dangerous confidence he exudes at times without more than anecdote to back it up, he’s taken feedback on these faults and later presentations are clarified to illustrate the doubt there is surrounding some ideas. I think he’s doing important work in considering new options and through conducting his own research. This is above and beyond what most doctors practicing medicine in clinic hold themselves responsible for, and I commend him for this drive toward excellence!
Estradiol (E2) is the primary female hormone (estrogen). It has the highest transactivational potential in cells where its receptors are expressed compared to other natural estrogens 1, and is secreted by the ovaries. 17β-Hydroxysteroid dehydrogenases (17β-HSD) are a group of enzymes involved in both steroid biosynthesis and metabolism. There are a variety of these isoforms that process varying sex steroids at differing preferentiality and efficiency. 2
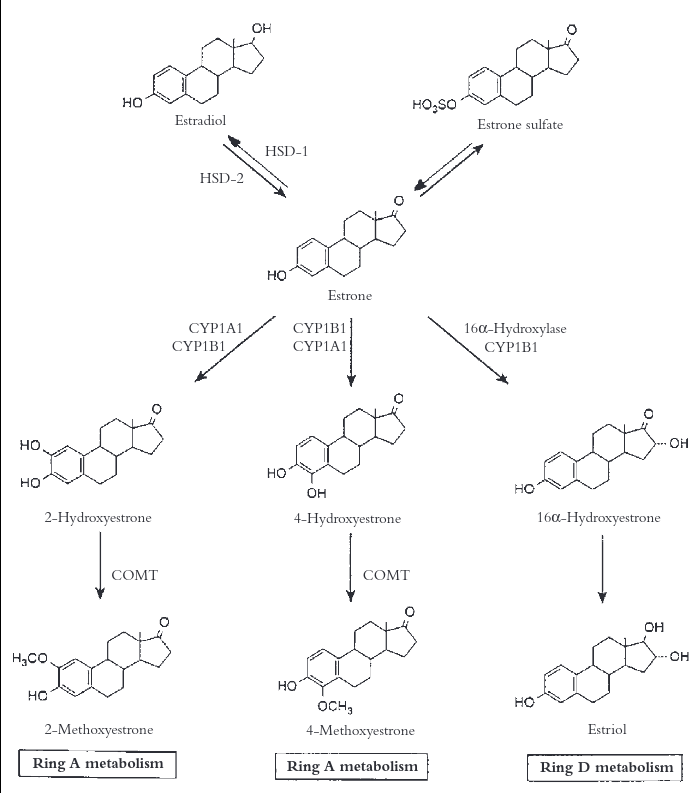
We see here that Type 1 catalyzes E1 into E2, whereas Type 2 performs the opposite process, metabolizing E2 into E1. Type 2 is abundantly expressed throughout the gastrointestinal tract, notably in the absorptive epithelium. 3 This explains the rapid metabolism commonly observed with the oral route of 17b-estradiol is employed in transfeminine hormone replacement therapy.
Oral administration of estradiol is by far the most commonly prescribed to trans girls, and as such, high daily doses are often necessary to obtain normal female levels. This comes at the expense of high circulating estrone, for which the potential consequences are the subject of much debate thanks to Dr. Powers. He has noticed in his transgender patients that about 50% of them exhibit an unexpectedly high proportion of E1 to E2, and speculates that this may impair feminization.
The majority of his patients are trans, and in the 7 years of facilitating and monitoring HRT, he has amassed a formidable amount of data he feels supports this claim. Yet, there is no formal research on effects of an abnormal ratio of E1:E2, in cis or trans persons, and he has yet to publish any of his data, either.
We could speculate on mechanisms by which this may happen. Maybe people could have genetic mutations affecting the structure of 17-HSD type 1/2 such that their activity is reduced or increased for estrogens, or perhaps a deficiency in the production of the liver enzymes that further metabolize estrone. There certainly exist many possible permutations of these, but further work to produce useful interpretations is still needed. 4
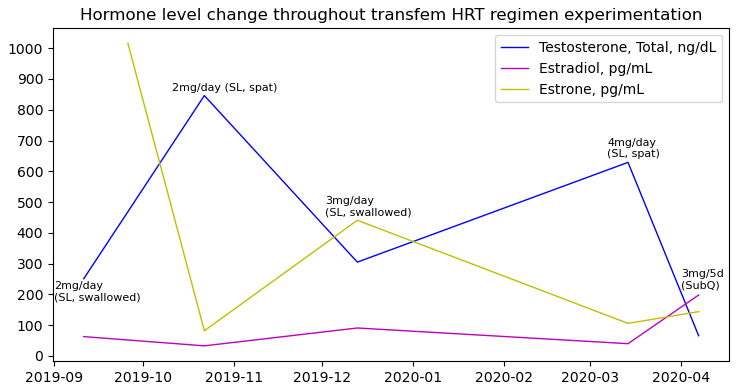
I started on sublingual estradiol to somewhat bypass this metabolism, hoping for better estradiol levels compared to oral, as a result. This didn’t happen. I was surprised to find my starting dose of 2mg daily resulted in rather low E2 levels at trough. This didn’t worry me, though. I wanted to mimic cisfem puberty, which is slow ramp up of E2 over years, and I thought this might actually be a good thing!
My initial prescriber at an informed consent clinic that I was seeing while waiting for my first appointment with an endocrinologist that my insurance covered couldn’t order estrone level testing. I ended up paying out of pocket for it by using the on demand lab ordering services LabsMD and PrivateMDLabs. Unfortunately, I found that I too had incredibly high levels - 5-10x that of E2.
Out of curiosity at first, I tried an experiment. Instead of swallowing the liquid after holding it under my tongue for 10-20 minutes, I’d spit it out. My hypothesis was that due to excess saliva, there was still a lot of estradiol that hit my intestines and were subject to 17b-HSD2 conversion to estrone. I tried this modified sublingual regimen consistently for a 2 week period and then had my blood drawn to see what happened! I allowed 22 hours to pass before turning my arm up in the phlebotomist’s chair and suffering her imprecision.
The results? Well, my hypothesis was certainly proven, but it also understandably caused E2 to drop. Astoundingly, E1 fell from over 1000pg/mL to 82pg/mL. Estradiol was only a measly 33pg/mL. Surprisingly, the ratio here is only a bit over 2:1. 17b-HSD2 expresses in the liver as well, so I wasn’t quite sure why the ratio was so low comparatively, if I did have a mutation.
Extrapolations I performed on pharmacokinetic graphs seemed consistent with my levels. See here and also here. These specifically were chosen as they most closely resemble the levels in which my labs are reporting and included twice daily dosing schedule.
| Time elapsed from dosing | Estimated serum level | Relative metabolism % to previous period |
|---|---|---|
| 1 hour | 2000pg/mL | |
| 2 hours | 700pg/mL | 65% |
| 3 hours | 400pg/mL | ~43% |
| 4 hours | 300pg/mL | ~25% |
| 6 hours | 200pg/mL | ~33% |
| 8 hours | 160pg/mL | ~20% |
| 10 hours | 140pg/mL | ~12.5% |
| 12 hours | 100pg/mL | ~29% |
After 4 hour mark, metabolism “slows” to an average 23% every 2 hours. This is likely caused by 17b-HSD1’s conversion of E1 into E2. Following values will be calculated based on this average.
| Time elapsed from dosing | Estimated serum level |
|---|---|
| 14 hours | 77pg/mL |
| 16 hours | 59pg/mL |
| 18 hours | 46pg/mL |
| 20 hours | 35pg/mL |
| 22 hours | 27pg/mL |
In retrospect, I probably let too much time pass between my last dose and the draw, but these things can be difficult to time. In any case, my T spiked enormously without pressure from estrone on the pituitary to reduce gonadal signaling. My anti-androgen couldn’t handle this massive increase, and I experienced involution. Back to to swallowing it was for me!
I went on like this for awhile, slowly raising my estradiol as breast development progressed. By the six month mark, I was at 4mg/day, and gave this experiment another shot. My reasoning here was that a higher dose may be sufficient to retain enough estrogenic activity to temper T to the point where my anti-androgen would remain effective.
To my despair, it still wasn’t enough! Again, I underwent involution, losing some breast mass and experiencing a sharp increase in libido and male-associated emotionality. To make matters worse, my breast development had stalled out for the last month.
I tried to get Lupron approved through my insurance, but was unsuccessful. It would have suppressed T completely at the gonadal level by inhibiting the signaling pathway upstream. That was a minor disappointment, but not unexpected, since its pretty well known that insurance won’t cover this anti-androgen for adults.
At this point, I decided to switch to injections. Initially, I was going to try for a small enough dose to continue to emulate puberty as closely as I could. In another odd and unexplainable moment where I nearly spit out my drink, follow up labs showed my E2 was at adult levels of 200pg/mL when using only 3mg every 5 days. Estradiol valerate does boast slower metabolism due its structure, but this was unusual, as I was taking half the typical starting dose. I have no satisfying explanation for why it played out like this for me…
…but my gender dysphoria had relented. My quality of life improved momentously! The persistent, low-grade depression I’d lived with for years lifted. My self-image improved to the point that I became comfortable outwardly presenting as a girl. I was no longer anxious about what people thought of me. My emotional understanding and expression became enriched. My priorities shifted after I reduced my dose and everything came crashing down around me. I had no idea what I had been missing out on and I badly wanted it back!
Having optimal breasts seemed like a silly thing to focus on by comparison, but by that metric, things had improved as well. They started growing again, and were on their way to filling out nicely. My estrone was controlled, albeit a bit low, but this didn’t especially bother me anymore. Not that there was anything I could especially do about it given how my body appears to process oral estradiol. I felt content for the first time in years, and that meant the world to me.
While this unconventional method of sublingual ROA didn’t work out for me, it might be effective for other trans girls. There is wide individualistic variation in metabolism and endogenous hormone levels. Perhaps this would work for someone who seeings higher levels of estrogens with HRT, or has naturally lower T! If you’re one of the lucky ones who are on a GnRHa, or get adequate suppression out of spironolactone, this seems like perfect way to control estrone.
-
Kuhl H. Pharmacology of estrogens and progestogens: influence of different routes of administration. Climacteric. 2005;8 Suppl 1:3-63. doi:10.1080/13697130500148875 ↩
-
Miller WL, Auchus RJ. The molecular biology, biochemistry, and physiology of human steroidogenesis and its disorders [published correction appears in Endocr Rev. 2011 Aug;32(4):579]. Endocr Rev. 2011;32(1):81-151. doi:10.1210/er.2010-0013 ↩
-
Sano T, Hirasawa G, Takeyama J, et al. 17 beta-Hydroxysteroid dehydrogenase type 2 expression and enzyme activity in the human gastrointestinal tract. Clin Sci (Lond). 2001;101(5):485-491. doi:10.1042/cs1010485 ↩
-
Moeller G, Adamski J. Integrated view on 17beta-hydroxysteroid dehydrogenases. Molecular and Cellular Endocrinology. 2009 Mar;301(1-2):7-19. doi:10.1016/j.mce.2008.10.040 ↩
« Anti-androgens: spironolactone and bicalutamide ✧ Choosing a smartphone in 2020 »